What is a Mammogram?

A mammogram is a breast-related X-ray image. This imaging procedure, which is highly popular, compresses and spreads out the breast using a device with two solid surfaces. The doctor can next check any anomalies in the black-and-white photographs of the breasts that were taken from two distinct angles. Mammography is the term for the collection of images that are taken of each breast. For the early identification of breast cancer, this gadget is employed.
Also read- How to measure blood pressure at home – My Biology Dictionary
Table of Contents
WHAT IS A BREAST CANCER?
Although skin cancer is the second most frequent cancer in women, males are nonetheless at risk for developing breast cancer. Male breast cancer accounts for a share of new cases each year, despite the fact that the percentage of cases is substantially lower than that of female breast cancer. Anyone could potentially develop the illness, regardless of gender, ethnicity, or race, especially if they have certain risk factors such as family history, genetics, or usage of oral contraceptives or hormones in the past.
Breast cancer is a condition in which the breast’s cells proliferate out of control. Breast cancer comes in several forms. Which breast cells develop into cancer determines the type of breast cancer Different areas of the breast might give rise to breast cancer. The ducts or lobules are where most breast cancers start.
Blood and lymph vessels are two ways that breast cancer can travel outside of the breast. Breast cancer is said to have metastasized when it spreads to other body regions.
HOW BREAST CANCER IS DETECTED?
Mammogram– An X-ray of the breast is what mammography is. Mammograms are frequently used as a breast cancer screening tool. Your doctor might advise diagnostic mammography if an abnormality is found on a screening mammogram in order to further assess that anomaly.
Ultrasound of breast– Ultrasound employs sound waves to create pictures of inside organs at great depths. If a new breast lump is found to be a solid mass or a cyst filled with fluid, an ultrasound may be performed to identify it.
Removing breast cells for testing and analysing (biopsy)-The only reliable technique to diagnose breast cancer is through a biopsy. Your doctor will perform a biopsy on the suspicious spot using a specialised needle instrument guided by an X-ray or other imaging test.
Magnetic resonance imaging of the breast (MRI)– A magnet and radio waves are used by an MRI machine to produce images of your breast’s interior. Depending on your circumstances, additional tests and treatments might be used.
Let us now learn more about the detection of breast cancers through mammography.
The test is crucial in detecting breast cancer at an early stage and lowering the number of deaths brought on by the disease. Examining any unusual lumps or growths in the breast tissue is also aided by it. The breasts are X-rayed using this screening method from top to bottom and from one side to the other. Diagnostic mammography, on the other hand, focuses on the problematic tissue or a specific lump. Mammography uses photographs of the patient’s breasts to look for tumours or other abnormalities in the tissue. It is an extremely effective method for finding breast tumours.
Screening mammography: This procedure looks for breast abnormalities in women who do not yet exhibit any symptoms or signs of breast cancer. The goal is to identify a malignant tumour before any clinical symptoms or indicators appear (early diagnosis).
Diagnostic mammography – This test is used to detect any suspicious breast changes, such as breast pain, lumps, strange skin colour, discharge from the nipples, an unusual breast form, thickening of the nipples, etc. Additional mammography images are included in a diagnostic mammogram.
The following are recommendations for getting a screening mammogram:
The average risk of breast cancer: Women often begin getting mammograms at the age of 40 and continue getting them every one to two years after that. The U.S. Preventive Task Force advises women to begin mammography at age 50 and to continue it periodically after that.
High risk of breast cancer: Women who have a suspected breast cancer risk can get screened before turning 40. The early detection of breast cancer will benefit from this. Additionally, if the woman’s family has a history of breast cancer, she may be at increased risk for the disease.
DIFFERENT TYPES OF MAMMOGRAPHY
Digital mammography, also known as full-field digital mammography (FFDM), is a type of mammography in which electronics, rather than x-ray film, are used to create mammographic images of the breast. These systems are comparable to those in digital cameras, and because of their effectiveness, it is possible to take better photographs with less radiation. The breast images are uploaded to a computer for the radiologist’s review and long-term archiving.
Computer-aided detection (CAD) systems look for anomalous areas of density, bulk, or calcification that could point to the presence of cancer on digitised mammographic pictures. The radiologist is informed to carefully examine these spots when the CAD system highlighted them on the images.
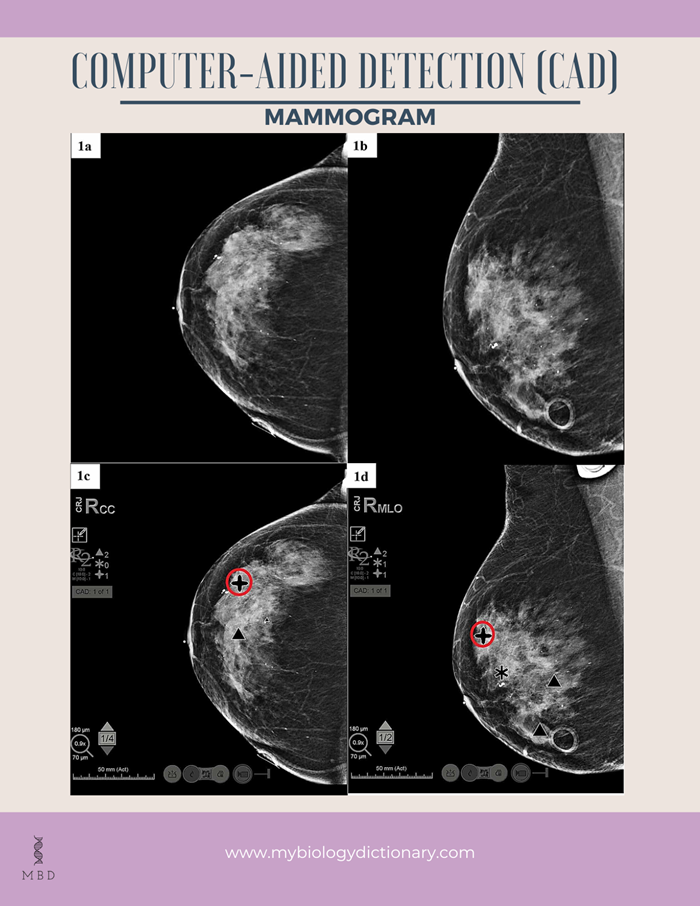
Image source: Rios, F. S., Movva, G., Movva, H., & Nguyen, Q. D. (2020). Current Available Computer-Aided Detection Catches Cancer but Requires a Human Operator. Cureus, 12(12).
Breast tomosynthesis, also known as digital breast tomosynthesis (DBT) and three-dimensional (3-D) mammography, is a sophisticated method of breast imaging that involves taking multiple images of the breast from various angles and reconstructing (or “synthesising”) them into a three-dimensional image set. Similar to computed tomography (CT) imaging, which assembles a number of thin “slices” to provide a 3-D reconstruction of the body, 3-D breast imaging uses light-emitting diodes (LEDs) to produce images of the breast
HOW IS THE MAMMOGRAM APPARATUS?
A mammography unit is a box with an x-ray tube inside. The device is only used for breast x-ray exams and has unique accessories to keep x-ray exposure to the breast to a minimum. The gadget in the unit holds and compresses the breast while positioning it so the technologist may take pictures from various perspectives.
Digital mammography systems are used to perform breast tomosynthesis, although not all of them have tomosynthesis imaging capabilities.
HOW DO WE OBTAIN THE RESULTS AND WHO INTERPRETS THEM? A radiologist, a medical professional qualified to oversee and interpret radiological exams, will review the pictures. Your primary care or referring physician will review the results with you after receiving a signed report from the radiologist. The mammography institution will also let you know the results.
A subsequent exam might be necessary. In that case, your physician will explain why. An additional examination or specialised imaging method may be used in a follow-up test to better assess a potential problem. Additionally, it might check to determine if a problem has changed over time. The best way to determine whether treatment is effective or whether an issue needs to be addressed is frequently through follow-up testing.
HOW RELIABLE IS A MAMMOGRAM?
Mammography has a 90% accuracy rate. The ability to find breast abnormalities before they grow large enough to be felt has improved because of mammograms. A mass you can feel, however, could not be visible on mammography. Your healthcare practitioner should examine any anomaly that you sense while feeling your breasts. They could advise getting diagnostic mammography.
WHAT CAN I ANTICIPATE FROM A MAMMOGRAM?
The steps involved in a mammogram are as follows:
- You must take off all clothing and jewellery that is visible above your waist. You will be given an open-front hospital gown or drape to wear by a caregiver.
- The mammography technologist will ask you to take one breast out of your gown at a time as you stand in front of the machine. Your breast will be placed on a breast support plate.
- The technician will press your breast against the support plate with a plastic paddle. During the 3- to 5-second compression period, you can experience some pressure or discomfort. Let the technician know if the pressure is too much for you, and they will make the necessary adjustments.
- As your breast is being crushed, an X-ray of it will be taken by the machine.
- You’ll repeat this procedure for your other breast if you have two.
- The operation will be finished once the technician has finished using the machine to take X-rays.
BENEFITS
Mammograms are a life-saving procedure.
By detecting breast cancer early, when it can be treated before growing or spreading to other regions of the body, screening mammograms save lives. Regular mammograms can lower your risk of breast cancer-related death by more than a third.
Possible reduction in treatment
Finding breast cancer early can result in less therapy being required than if it were discovered later and had already spread to other body areas.
A tested technique for detecting cancer
Mammograms can detect 8 to 9 out of 10 malignancies in women between the ages of 45 and 69. Even between mammograms, it’s crucial to keep an eye out for any changes in your breasts and to discuss them with your doctor right once.
Every two years, eligible women between the ages of 45 and 69 can receive complimentary mammography. We will send you an appointment time as soon as you sign up, and you will receive a reminder every two years.
DANGERS AND RISKS
Not all tumours are detected by mammograms.
Even if there is cancer present in the breast someplace, mammography may appear normal. About 1 or 2 out of 10 malignancies in women between the ages of 45 and 69 are not detected by mammography.
Radiation
You are exposed to a little amount of radiation during a mammogram because it is an X-ray, but this radiation is unlikely to be harmful. Digital mammograms use even less radiation than traditional mammography.
Pain and anxiety
For some women, a mammogram can be uncomfortable or even painful, and it can also cause worry and anxiety.
To summarize, a mammogram is an X-ray picture of the breast and it can be used by doctors to diagnose various conditions. We must appreciate the advancement of medical technologies and at the same time be aware of the cons.
Keep reading
Team MBD
Watch here- (1) Let’s Talk Mammograms – YouTube






nicely explained& good content….
Nice👍💕